- Leinweber J, Fonstein-Kuipers Y, Thomson G, Karlsdottis S, Nilsson C, Ekström-Bergström A, Olza I, Hadijigeorgiou E, Stramrod C. Developing a woman-centred, inclusive definition of traumatic childbirth experiences. In21st International Normal Labour and Birth Research Conference Denmark–Aarhus 2022. September 12th to 14th 2022 2022 (pp.1).
- Wojcieszek AM, Bonet M, Portela A, Althabe F, Bahl R, Chowdhary N, Dua T, Edmond K, Gupta S, Rogers LM, Souza JP, Oladapo OT. WHO recommendations on maternal and newborn care for a positive postnatal experience: strengthening the maternal and newborn care continuum. BMJ Glob Health. 2023 Jan;8(Suppl 2):e010992. doi: 10.1136/bmjgh-2022-010992. PMID: 36717156; PMCID: PMC9887708
- Tsakmakis PL, Akter S, Bohren MA. A qualitative exploration of women’s and their partners’ experiences of birth trauma in Australia, utilising critical feminist theory. Women and Birth. 2023 Jul 1;36(4):367-76.
- Watson K, White C, Hall H, Hewitt A. Women’s experiences of birth trauma: A scoping review. Women and Birth. 2021 Sep 1;34(5):417-24.
- Sun X, Fan X, Cong S, Wang R, Sha L, Xie H, Han J, Zhu Z, Zhang A. Psychological birth trauma: A concept analysis. Frontiers in Psychology. 2023 Jan 13;13:1065612.
- Vignato J, Georges JM, Bush RA, Connelly CD. (2017). Post-traumatic stress disorder in the perinatal period: A concept analysis. J Clin Nurs. 26: 3859–3868. https://doi-org.ezproxy.ecu.edu.au/10.1111/jocn.138002.
- Horsch A, Garthus-Niegel S, Ayers S, et al. Childbirth-related posttraumatic stress disorder: definition, risk factors, pathophysiology, diagnosis, prevention, and treatment. American journal of obstetrics and gynecology. 2024;230(3S):S1116-S1127. doi:10.1016/j.ajog.2023.09.089
- Bingham, J., Kalu, F. A., & Healy, M. (2023). The impact on midwives and their practice after caring for women who have a traumatic childbirth: A systematic review. Birth, 50(4), 711-734.
- Öz, Beyza, and Dilara Eren. n.d. “Midwifery Students’ Traumatic Childbirth Experiences, Traumatic Childbirth Perceptions, and Levels of Fear of Childbirth.” Journal of Midwifery & Women’s Health 68 (2): 248–54. https://doi.org/10.1111/jmwh.13464.
- Fontein-Kuipers Y, Duivis H, Schamper V, Schmitz V, Stam A, Koster D. Reports of work-related traumatic events: a mixed-methods study. Eur J Midwifery. 2018; 2: 18.
- Leinweber J, Creedy DK, Rowe H, Gamble J. Responses to birth trauma and prevalence of posttraumatic stress among Australian midwives. Women Birth. 2017; 30(1): 40-45.
- Toohill J, Fenwick J, Sidebotham M, Gamble J, Creedy DK. Trauma and fear in Australian midwives. Women Birth. 2019; 32(1): 64-71.
- Rice H, Warland J. Bearing witness: midwives experiences of witnessing traumatic birth. Midwifery. 2013; 29(9): 1056-1063.
- Sheen K, Spiby H, Slade P. Exposure to traumatic perinatal experiences and posttraumatic stress symptoms in midwives: prevalence and association with burnout. Int J Nurs Stud. 2015; 52(2): 578-587.
- Yilmaz Sezer, N., Aker, M. N., Öz, B., & Eren, D. (2023). Midwifery Students’ Traumatic Childbirth Experiences, Traumatic Childbirth Perceptions, and Levels of Fear of Childbirth. Journal of Midwifery & Women's Health, 68(2), 248-254.
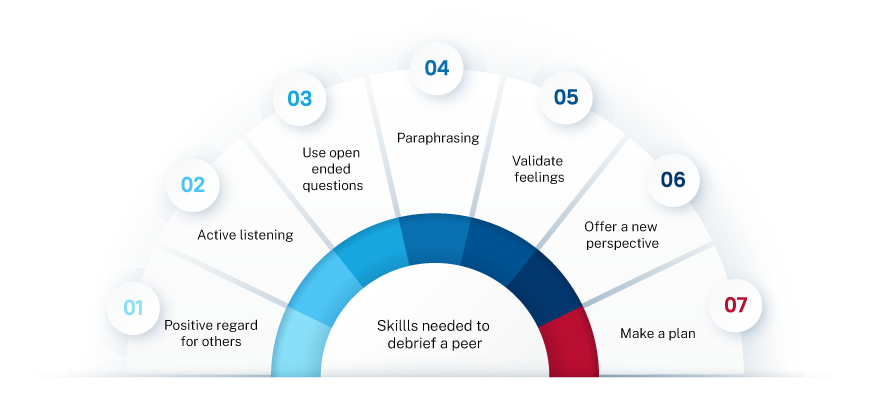
- Buchanan, K., Ross, C., Bloxsome, D., Hocking, J., & Bayes, S. (2024). Development of a midwifery student peer debriefing tool: An interpretive descriptive study. Nurse Education Today, 137, 106167.
- Gamble, J., Creedy, D., & Moyle, W. (2004). Counselling processes to address psychological distress following childbirth: perceptions of midwives. Australian Midwifery, 17(3), 16-19.
- Farber, B. A., Suzuki, J. Y., & Lynch, D. A. (2018). Positive regard and psychotherapy outcome: A meta-analytic review. Psychotherapy, 55(4), 411.
- Alves, S. P., Costa, T., Ribeiro, I., Néné, M., & Sequeira, C. (2023). Perinatal mental health counselling programme: A scoping review. Patient Education and Counseling, 106, 170-179.
- Doas, M. (2015). Are we losing the art of actively listening to our patients? Connecting the art of active listening with emotionally competent behaviours. Open Journal of Nursing, 5(06), 566.
- Östlund, A. S., Wadensten, B., Häggström, E., Lindqvist, H., & Kristofferzon, M. L. (2016). Primary care nurses' communication and its influence on patient talk during motivational interviewing. Journal of advanced nursing, 72(11), 2844-2856.
- Adanna, C. M., & Olumide, O. (2023). Counselling Skills for Effective Counselling in Schools. Journal of Innovation in Education and Social Research, 1(3), 208-215.
- Thomas, C. (2022). Coaching and mentoring skills: a complement to the professional midwifery advocate role. British Journal of Midwifery, 30(5), 290-296.
- Aktas, S., & Pasinlioğlu, T. (2021). The effect of empathy training given to midwives on the empathic communication skills of midwives and the birth satisfaction of mothers giving birth with the help of these midwives: A quasi‐experimental study. Journal of evaluation in clinical practice, 27(4), 858-867.
- Cummins, Allison M., Raechel Wight, Nicole Watts, and Christine Catling. n.d. “Introducing Sensitive Issues and Self-Care Strategies to First Year Midwifery Students.” Midwifery 61: 8–14. https://doi.org/10.1016/j.midw.2018.02.007.
- Seelandt, J. C., Walker, K., & Kolbe, M. (2021). “A debriefer must be neutral” and other debriefing myths: a systemic inquiry-based qualitative study of taken-for-granted beliefs about clinical post-event debriefing. Advances in Simulation, 6, 1-15.
- About ECU
Welcome to ECU
ECU offers innovative and practical courses across a variety of disciplines and we have a vibrant research culture. ECU is a leader in developing alternative entry pathways to higher education.
- Continue on to About ECU
Our campusesWe have three campuses in Western Australia. Joondalup and Mount Lawley in the Perth metropolitan area and our South West campus in Bunbury, 200km south of the Perth CBD.
Campus facilitiesECU provides a variety of services and facilities that go beyond the classroom, with opportunities for personal development and social interaction for students and staff.
- Study
Browse courses by study area
- Arts & Humanities
- Business & Law
- Engineering & Technology
- Medical & Health Sciences
- Nursing & Midwifery
- Science
- Teacher Education
- Western Australian Academy of Performing Arts
- Course entry
- Fees and scholarships
- Applying for courses
- Early Offer Program
- Mid-Year study
- Year 12 Pathways
- Important dates
- Events for future students
- Life on campus
- Short courses
- Continue on to Study
Browse courses by study typeInternational studentsContact usIn Australia
International
- Research
Our Research
At ECU we concentrate our research in areas of strength to deliver tangible outcomes.
- Continue on to Research
How to get involvedThere are several ways to get involved with research at ECU.
Graduate researchECU has a lively research community that is committed to supporting research students.
Supporting researchersResearch Services provides comprehensive support services to researchers.
- Industry
Research
We value industry partnerships and offer access to world-class research across our nine ECU Strategic Research Institutes and Centres.
ECU links our stakeholders to our professional talent pool across a range of disciplines and research topics.
- Continue on to Industry
Partner with usWe collaborate with all types of businesses, including new start-ups, small to medium enterprises, not-for-profits, community organisations, government and large corporates in the resources sector.
Professional developmentECU delivers training that can be tailored to industry needs.
Extra-curricular learning for childrenChildren's University Edith Cowan aims to inspire students between seven and fourteen to develop confidence and a love of learning through validated activities beyond the school curriculum.
Contact our team- Call us on 134 328
- Complete our enquiry form
- Alumni and Supporters
Inspiring Minds Scholarships Fund
The Inspiring Minds scholarship program are equity scholarships that give students an opportunity to access an education that may otherwise be out of reach.
EventsCatch up with fellow graduates at one of our regular alumni events.
- Continue on to Alumni and supporters
Get involvedWe love to see our graduates back at ECU helping current students achieve their dreams.
Stay in touchTell us what you've been up to since you graduated or stay in the alumni loop.
Professional developmentTake advantage of a range of career development or other alumni benefits.